Introduction
ATP is released into the extracellular milieu upon cell and tissue damage, secretory exocytosis or activation of plasma membrane transporters.
Many types of excitatory or non-excitatory cells maintain specific receptors to ATP or other nucleotides on their surface. Nucleotide receptors, also named P2, in contrast to P1 adenosine receptors, comprise two different families: ionotropic P2X receptors and metabotropic P2Y receptors.
P2X receptors
P2X receptors bear a common topology, containing intracellular N- and C- termini, two transmembrane domains and a large, usually glycosylated, extracellular loop, which contains 10 conserved cysteines. The topology is similar to that of the ENaC/ASIC superfamily. Like other ion channels, the functional channel is formed by homo- or hetero-oligomeric assembly of several subunits. The stoichiometry of the assembly is unknown.
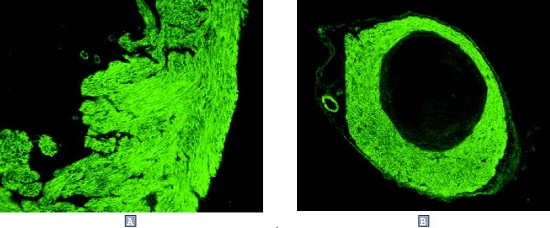
To date, seven distinct P2X receptors, named P2X1-P2X7, have been identified at the molecular level. These channels differ in their sensitivity to ATP and different ATP analogs, as well as in inactivation kinetics. The binding of extracellular ATP leads to the opening of nonselective cation channel, permeable to Ca2+. Prolonged exposure of slowly inactivating isoforms with ATP leads to dilation of the pore5, 6, making it permeable to larger molecules. The physiological relevance of pore dilation is unclear, except for the non-desensitizing P2X7, whose function is mediated by both Ca2+ permeation and its permeability to molecules with molecular weight up to 900 Da.7 P2X1 receptor is the dominant P2X type in smooth muscle cells1. Targeted disruption of P2X1 gene in mice leads to male infertility due to inability of vas deferens smooth muscle cells to contract2. This illustrates an important role of ATP as a neuromediator, which is co-released with noradrenaline from sympathetic nerves. Interestingly, while P2X1 is highly expressed in blood platelets3, its disruption in mice does not lead to any bleeding disorder2. In humans, however, a dominant negative mutation of P2X1 gene leads to a severe bleeding disorder due to an impairment of ADP-induced platelet aggregation4.
Most types of P2X receptors are distinctly distributed in peripheral and central neurons. Among them, P2X3 expression is restricted to a subpopulation of sensory neurons, which are positive for staining with a specific lectin, IB4, and express capsaicin receptors8,9. Since ATP, released due to tissue damage, can evoke a sensation of pain11, a specific role in the sensing of damage (nociception) has been suggested for this isoform. Indeed, mice lacking P2X3 receptor were less sensitive to pain-producing stimuli, as well as to nonnoxious warming (<45°C)11,12. Surprisingly, P2X3 appeared to transduce a sensation of urinary bladder pressure, most probably mediated by ATP released from urothelium by stretch11.
In other sensory neurons, sensory signals are mediated by P2X2/P2X3 heterooligomers31-33. P2X4 and P2X6 receptors are highly expressed in the central nervous system, possibly forming functional heterooligomers30. Their functional role remains to be elucidated. In vascular endothelium, shear stress leads to the release of ATP into the blood flow. P2X4, which is expressed in the vascular endothelium, seems to be involved in the shear stress-mediated Ca2+ influx28,29.
The P2X7 (P2Z) receptor is expressed in the cells of immune and hematopoetic origin. It is not expressed in monocytes, but appears when they differentiate to macrophages, and is highly upregulated by the stimuli that activate macrophages13. It is involved in a variety of functions, such as cytotoxicity, formation of multinucleated giant cells, antigen presentation, and, especially, IL-1 secretion14,27. P2X7 is also expressed in microglial cells15.

P2Y receptors
The metabotropic P2Y receptors are part of the 7 TM G-protein coupled receptor superfamily. The current nomenclature of P2Y receptors has been based solely on the chronology of the cloning. As recommended by IUPHAR, the term P2Y is used for a cloned receptor which has been proven to mediate effects of extracellular nucleotides. The lower case, p2y, is used for cloned receptors, whose function as nucleotide receptors has not been shown17,34. In some cases, the receptors have been prematurely designated p2y, while their sensitivity to nucleotides has not been proven. The p2y7 receptor is, in fact, a leukotriene B4 receptor, whereas the p2y5, p2y9 and p2y10 receptors must be considered as orphan receptors.
Genuine functional P2Y receptors can be clustered into three groups:
- Selective purinoceptors (P2Y1 and P2Y11).
- Selective pyrimidinoceptors (P2Y6).
- Receptors of mixed selectivity-(P2Y2 and P2Y4).
All cloned and functionally expressed P2Y receptors couple to phospholipase C, leading to the breakdown of phosphoinosi tide to inositol 1,4,5-phosphate (InsP3) and diacylglycerol, and InsP3-dependent increase in cytosolic Ca2+ concentration. In addition, P2Y11 couples to the adenylate cyclase pathway.24
P2Y1 is widely distributed. In blood platelets, it is responsible for their initial shape change in response to ADP20. The platelets from P2Y1-knockout mice are unable to aggregate in response to standard concentrations of ADP. These mice are resistant to thromboembolism induced by intravenous injection of ADP, collagen or adrenaline21,22.
Another adenylate cyclase-coupled receptor called P2TAC, P2CYC or P2YADP is responsible for later ADP-dependent amplification of platelet aggregation and thrombus stabilization. The recently cloned orphan G protein coupled receptor SP1999 seems to be a candidate for this role23. In the airways, the volume and composition of liquid secretions are regulated by extracellular ATP or UTP35. P2Y2 receptor, expressed in epithelial cells, is linked to Ca2+-activated Cl– channel36. Since the latter may provide a Cl– conductance, distinct from that mediated by cystic fibrosis transmembrane conductance regulator (CFTR), P2Y2 has been suggested as a potential target for therapy of cystic fibrosis lung disease37-39.
Interestingly, in P2Y2 (-/-) mice, the nucleotide-dependent Cl– channel was almost completely absent in airways epithelium, but remained unimpaired in the intestines25.
P2Y11 mediates ATP-dependent white cell differentiation of several leukemia-derived cell lines26.
The current knowledge on the function of P2Y receptors in different tissues is still far from complete. The list of cloned P2Y receptors may also be incomplete. The high diversity of this group in comparison to other families of G protein coupled receptors makes it more difficult to identify new P2Y receptors6.

*According to other reports, ATP is a weak agonist of P2Y118.
**For rP2Y4 and tp2y, UTP=ATP19.
Abbreviations: c, chicken; t, turkey; b, bovine; m, mouse; r, rat; x, Xenopus.
References
- Vulchanova, L. et al. (1996) Proc. Natl.Acad.Sci. USA 93, 8063.
- Mulryan, K. et al. (2000) Nature 403, 86.
- Scase, T.J. et al. (1998) Biochem. Biophys. Res. Commun. 242, 525.
- Oury, C. et al. (2000) J. Biol. Chem. 275, 22611.
- Virginio, C. et al. (1999) Nat. Neurosci. 2, 315.
- Virginio, C. et al. (1999) J. Physiol. 519, 335.
- Surprenant, A. et al. (1996) Science. 272, 735.
- Guo, A. et al. (1999) Eur. J. Neurosci. 11, 946.
- Bradbury, E.J. et al. (1998) Mol. Cell. Neurosci. 12, 256.
- Bleehen, T. and Keele, C.A. (1977) Pain 3, 367.
- Cockayne, D.A. et al. (2000) Nature 407, 1011.
- Souslova, V. et al. (2000) Nature 407, 1015.
- Di Virgilio, F. (1995) Immunol. Today 16, 524.
- Di Virgilio, F. et al. (1999) J. Leukoc. Biol. 66, 723.
- Mutini, C. et al. (1999) J. Immunol. 163, 1958.
- Di Virgilio, F. et al. (1999) Prog. Brain. Res. 120, 355.
- King, B.F. et al. (1998) Trends Pharmacol. Sci. 19, 506.
- Palmer, R.K. et al. (1998) Mol. Pharmacol. 54, 1118.
- Bogdanov, Y.D. et al. (1998) Br. J. Pharmacol. 124, 428.
- Kunapuli, S.P. (1998) Trends. Pharmacol. Sci. 19, 391.
- Leon C. et al. (1999) J. Clin. Invest. 104, 1731.
- Fabre, J.E. et al. (1999) Nat. Med. 5, 1199.
- Zhang, F.L. et al. (2001) J. Biol. Chem., in press.
- Communi, D. et al. (1997) J. Biol. Chem. 272, 31969.
- Cressman, V.L. et al. (1999) J. Biol.Chem. 274, 26461.
- van der Weyden, L. et al. (2000) Immunol. Cell. Biol. 78, 369.
- Solle, M. et al. (2001) J. Biol. Chem. 276, 125.
- Yamamoto, K. et al. (2000) Am. J. Physiol. 279, H285.
- Yamamoto, K. et al. (2000) Circ. Res. 87, 385.
- Le, K.T. et al. (1998) J. Neurosci. 18, 7152.
- Virginio, C. et al. (1998) J. Physiol. 510, 27.
- Burnstock, G. (2000) Br. J. Anaesth. 84, 476.
- Tsuda, M. et al. (2000) J. Neurosci. (Online) 20, RC90.
- von Kuegelgen, I, and Wetter, A (2000) Naunyn-Schmiedebergs Arch. Pharmacol. 362, 310.
- Mason, S.J. et al. (1991) Br. J. Pharmacol. 103, 1649.
- Hwang, T.H. etal. (1996) Am. J. Physiol. 270, C1611.
- Knowles, M.R. et al. (1991) N. Engl. J. Med. 325, 533.
- Williams, M. (1996) Ciba Found. Symp. 198, 309.
- Agteresch, H.J. et al. (1999) Drugs 58, 211.
- Hollopeter, G. et al. (2001) Nature 409, 202.